Introduction
Immobilization gives a comfortable and relaxed patient position in order to improve setup accuracy. Therefore, it is highly preferred in precision radiotherapy to deliver treatment with accuracy and reproducibility.
IMRT and 3D-CRT treatments are successful, only if, the treatment is done with proper immobilization.
The Main Objective of immobilization
Reduce the probability of major positioning errors
- Stabilize the relation between external skin markers and internal structures
- Identify treatment position for post-irradiation imaging
- Give a sense of more secure and less apprehensive feeling to the patient.
- Limit the patient motion
- Reduce time for daily patient setup
Immobilization devices
- The thermoplastic
- Vacuum cushion system
- Organ immobilization
- Stereotactic frames: Brown-Roberts-Wells device
- Base plate
- Foot separation device
- Head support Bite block
- Shoulder retraction
- Hand grips Arms support.
The devices should be compatible with simulator or CT scan and should not produce any image artefacts.
The thermoplastic and vacuum cushion system are the most popular, and the thermoplastic used in head and neck region is usually called as facial masks
Thermoplastic Device
The thermoplastic device is the cheapest and easy to use technology.
It is basically a nontoxic thermoplastic compound, which has been analytically tested for non-allergic testing.
They have less shrinkage and would not stick to the patient skin or hair. It is available either with perforation or non perforation of varying thickness from to 3.2 mm.
It is also available in standard as well as precut design, for both adults and pediatric use.
Thermoplastic Mask Preparation in Radiation Therapy
A precut design is in the form 2.3.4. and 5 clamps, to suit an individual patient.
To make a patient mask, a microprocessor controlled water bath is required and the suitable heating temperature is about 70°C.
During the course of treatment, the patient may lose weight and the mask may need adjustment.
Thermoplastic shells are easy to adjust locally with the help of heating gun, and it is their advantage over clear plastic shells

Bite Block
Bite block is used to keep the mouth open during treatment, along with external masks.
It not only keeps the mouth open but also restricts the tongue motion.
It is usually made with wax or dental impression compound. The wax or dental material is heated initially and then shaped around a hollow plastic tube.
Klarity EasyBite Bite Block (RKY-01)
Effective, Easy to use, Cost effective,
- The bite block molds into the mask easily
- Thermoplastic attachment is moldable for precisely confirming to the teeth, which provides best stability
- Dual airway for patient’s easy breathing
- Easy for therapist to use with handle
The patient is asked to bite the material and the impression of the teeth is obtained. Later, it cools down and becomes hard.
The plastic hollow tube ensures that the patient’s air pathway is not blocked.
There is need to disinfects the bite block after each use.
Nowadays, bite blocks are available commercially, which can be attached to the external thermoplastic mask.
This will avoid the rotation and flexion movements, while pressing the tongue.
Mask Making Process
Position the patient with a suitable base plate head rest
Place the thermoplastic precut into the water heater for about 1-2 minutes or up to 70°C.
Take it out and shake gently to remove the excess water
Place the mask centrally on the body part of the patient Tilting slightly downward, gently press the thermoplastic towards the patient skin, until the edges touch the base plate
Press the entire surface of the thermoplastic, so that it takes the shape of the patient contour
Allow it to cool for about 5 minutes or until it becomes white Remove it from the patient, and write the patient’s name and hospital number.
Vacuum Cushion System
The vacuum cushion is made up of nylon and filled with small polystyrene spheres .
The nylon gives rigidness, prevents puncture and leaks and provides longer life.
The patient is positioned on the cushion and the air is evacuated with an vacuum pump, Now, the cushion becomes rigid and can be used until the treatment is
completed.
It is air tight
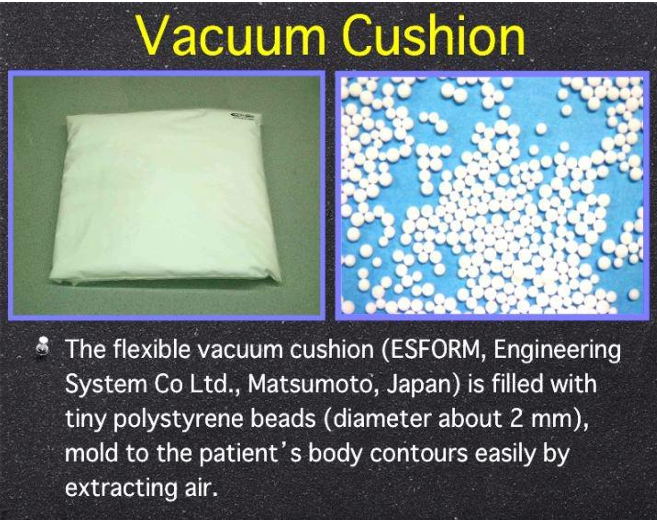
durable, reusable and cost effective. It suits a variety of treatment fields and are available in various sizes: 20 x 25 cm, 70 x 50 cm.100 x 60 cm and 120×80 cm
It is also available in the form of body cushion, head and neck cushion, pelvic cushion, etc. and can be used even without base plate.
Usually, vacuum cushions are purchased with set of two-way vacuum pump and cushion stand with S cooks
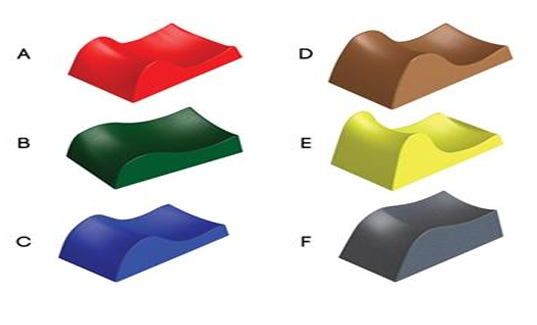
Head Rests
HR are made up of acrylic material or polyurethane foar or carbon fiber.
Six sizes of head rest are there to suit different elevation contours of the patient for a given treatment

They are marked asA,B,C,D,E and F easy identification.
Head rest offers minimal skin reaction and has negligible beam attenuation
Breast and thorax base plate Abdomen and pelvic boards.
They are basically made up of acrylic or carbon fibre material, has minimal attenuation, adjustable arm supports and CT compatible.
They are light weight and indexable to any couch Head and neck base plate is available as tilting base plate, prone head holder and lateral base plate
Belly board is especially used to remove small bowel from the treatment field with the use of three interchangeable.
Breast board
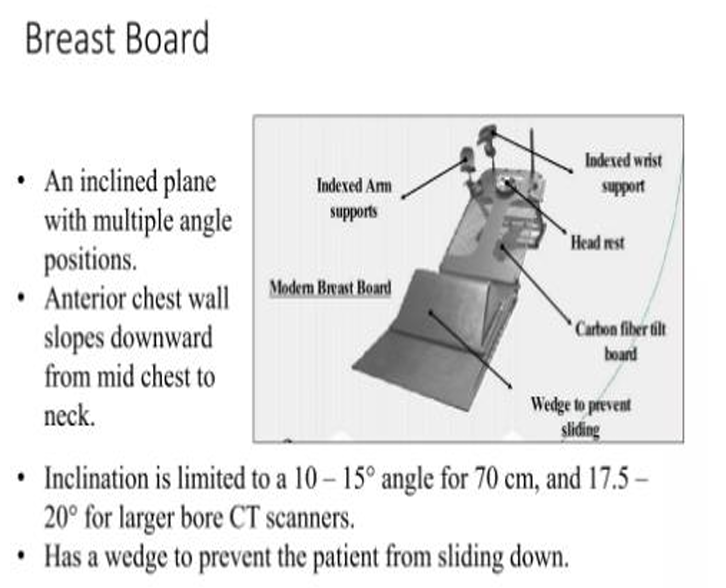
Advantages of Breast board
Several adjustable parts to allow for the manipulation of patient’s arms, wrists, head & elevation.
Makes chest wall surface horizontal
Takes the arms out of the way of lateral beams
thermoplastic breast support can be added for immobilization of large pendulous breast.
Constructed of carbon fibre which has lower attenuation levels permitting beam penetration
Prone breast board
System includes
- prone board
- face cusion
- 15 degree contralateral wedge
- handles
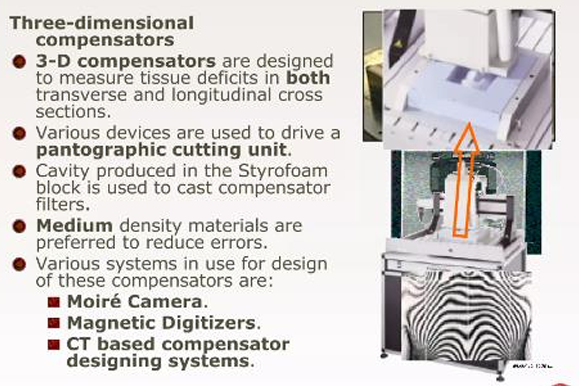
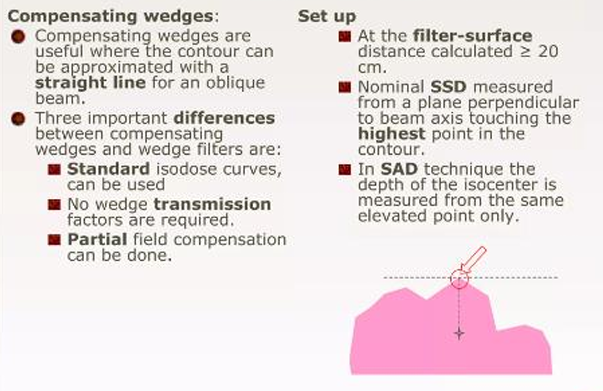
Compensators
A beam modifying device which evens out the skin surface contours, while retaining the skin sparing advantage
it allows normal depth dose data to be used for such irregular surfaces.
compensators can also be used for
- to compensate for tissue heterogeneity this was first used by Ellis, and is primarily used in total body irradiation
- to compensate for dose irregularities arising due to reduced scatter near the field edges (example mantle fields), and horns in the beam profile.
The dimension and shape of a compensator must be adjusted to account for
- Beam Divergence
- linear attenuation coefficients of the filter material and soft tissue
- Reduction in scatter at various depths due to the compensating filters, when it is placed at the distance away from the skin
To compensate for these factors a tissue compensator is always has an attenuation less than that required for primary radiation
As the distance between the skin and compensator increases the thickness ratio decreases.
The thickness ratio depends on
- compensator to surface distance
- Thickness of the missing tissue
- Field size
- Depth
- Beam quality
of these the distance is the most important factor when d is less than equal to the 20 cm
Therefore, a fixed value of thickness ratio is used for most compensator work (~0.7)
The formula used for calculation of compensator thickness is given by TD x T/Pc where TD is the tissue deficit and Pc is the density of the compensator
the term T/Pc can be directly measured by using phantoms
The term compensator ratio is the inverse of the thickness ratio (Pc/t)